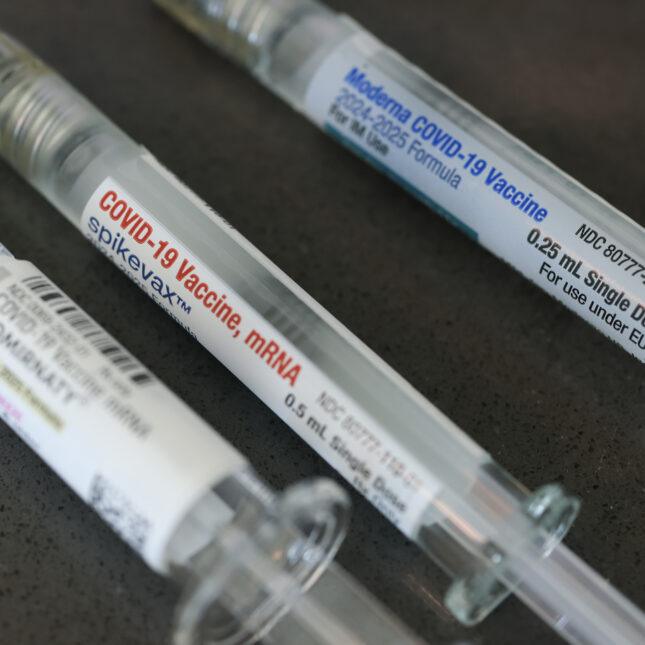
Study Suggests mRNA COVID-19 Vaccines May Enhance Cancer Immunotherapy Effectiveness
October 2025 — A groundbreaking new study has revealed that mRNA COVID-19 vaccines — originally developed to protect against the coronavirus — may also boost the effectiveness of cancer immunotherapy treatments. The research, conducted by scientists at multiple international institutions, highlights how vaccine-induced immune activation could improve the body’s ability to recognize and destroy cancer cells & a recent study published in MD Anderson Cancer center
How COVID-19 Vaccines Could Help Cancer Treatment
According to findings published this week in Nature Medicine, researchers discovered that the mRNA technology used in COVID-19 vaccines can stimulate key immune pathways that overlap with those targeted by cancer immunotherapy drugs. Specifically, the vaccines appear to enhance the activity of T cells, the immune system’s front-line defenders responsible for detecting abnormal or malignant cells.
Dr. Lina Ortega, lead immunologist at the University of Cambridge and one of the study’s authors, explained that the results suggest an unexpected synergy between pandemic-era vaccine innovation and cancer treatment progress.
“Our data indicate that mRNA vaccines may act as an immune ‘primer,’ improving responsiveness to certain immunotherapies,” Dr. Ortega said. “This could open an entirely new frontier in personalized cancer care.”
The team studied over 1,200 cancer patients receiving checkpoint inhibitor therapies between 2021 and 2024. Those who had received at least two doses of an mRNA COVID-19 vaccine demonstrated higher treatment response rates and longer progression-free survival compared to unvaccinated patients.
Immune System “Reprogramming” Through mRNA Technology
The mRNA platform, used in Pfizer-BioNTech and Moderna COVID-19 vaccines, teaches cells to produce harmless viral spike proteins, triggering an immune response. Researchers now believe that the same mechanism might “train” the immune system to become more alert to other abnormal cells — including cancer cells.
In the new study on mRNA COVID-19, scientists found elevated levels of interferon-gamma and cytotoxic T cells, immune markers associated with tumor destruction, in vaccinated patients. The immune system appeared to remain in a heightened state of readiness, which enhanced the effects of cancer immunotherapies designed to unleash immune cells against tumors.
Dr. Marcus Heller, an oncologist at the Dana-Farber Cancer Institute who was not involved in the study, described the findings as “exciting and biologically plausible.”
“mRNA COVID-19 vaccines seem to provide a short-term boost to immune surveillance,” Heller noted. “When combined with immunotherapy drugs, that heightened immune vigilance may translate into better tumor control.”
Potential Game Changer for Cancer Immunotherapy
Immunotherapy, particularly the use of checkpoint inhibitors such as pembrolizumab and nivolumab, has revolutionized treatment for melanoma, lung cancer, and several other malignancies. However, only a subset of patients responds effectively — often because the immune system fails to recognize cancer cells as threats.
The new findings suggest that mRNA-based immune activation could help overcome this limitation. Researchers are now exploring whether tailored mRNA vaccines could be developed specifically to enhance cancer therapy outcomes.
Some companies, including BioNTech and Moderna, have already begun clinical trials combining mRNA vaccines with existing cancer drugs, targeting tumors such as melanoma and pancreatic cancer. The latest results lend additional weight to this strategy, potentially accelerating future approvals.
Safety and Future Research
While the data are promising on mRNA COVID-19, scientists caution that more research is needed to fully understand how long the immune-enhancing effect lasts and whether it applies across all cancer types. The study found no increase in severe side effects among vaccinated cancer patients, supporting the safety of mRNA vaccines even for those with compromised immune systems.
“We want to emphasize that this doesn’t mean everyone with cancer should get extra vaccine doses without medical guidance,” Dr. Ortega added. “But it does highlight how mRNA technology could be repurposed beyond infectious diseases.”
Future investigations aim to identify the optimal timing between vaccination and immunotherapy sessions, as well as the molecular mechanisms behind the observed synergy.
Broader Implications for mRNA Medicine
Beyond oncology, these findings strengthen optimism about mRNA as a versatile therapeutic platform. The technology, once seen as experimental, has now proven adaptable for infectious diseases, genetic disorders, and now — potentially — cancer immunotherapy enhancement.
Pharmaceutical analysts predict that by 2030, mRNA-based cancer vaccines could represent a multibillion-dollar market, as personalized medicine becomes central to modern oncology.
“The pandemic inadvertently fast-tracked mRNA science by nearly a decade,” said Dr. Heller. “We’re now seeing that momentum ripple through every area of medical research, from viruses to cancer.”
Public Health Significance
Experts believe this discovery may also help reduce vaccine hesitancy among cancer patients, who were initially cautious during the pandemic. If future trials confirm the dual benefits of mRNA vaccination — protection from COVID-19 and improved cancer treatment outcomes — public health campaigns may incorporate this evidence to encourage vaccination within vulnerable populations.
As Dr. Ortega concluded:
“The intersection between infectious disease research and oncology is one of the most exciting developments in modern medicine. What started as a tool to fight a global pandemic could soon become a weapon in the fight against cancer.”